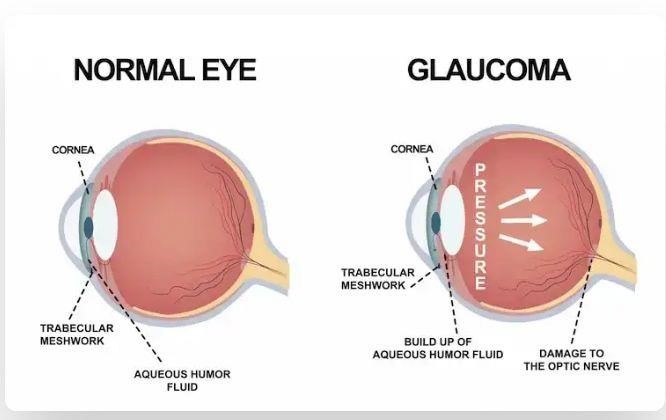
Glaucoma is a condition that damages your eye’s optic nerve. It gets worse over time. It’s often linked to a buildup of pressure inside your eye.
Glaucoma tends to run in families. You usually don’t get it until later in life.
The increased pressure in your eye, called intraocular pressure, can damage your optic nerve, which sends images to your brain. If the damage worsens, glaucoma can cause permanent vision loss or even total blindness within a few years.
Most people with glaucoma have no early symptoms or pain. Visit your eye doctor regularly so they can diagnose and treat glaucoma before you have long-term vision loss.
If you lose vision, it can’t be brought back. But lowering eye pressure can help you keep the sight you have. Most glaucoma patients who follow their treatment plan and have regular eye exams can support their vision.
Glaucoma Causes
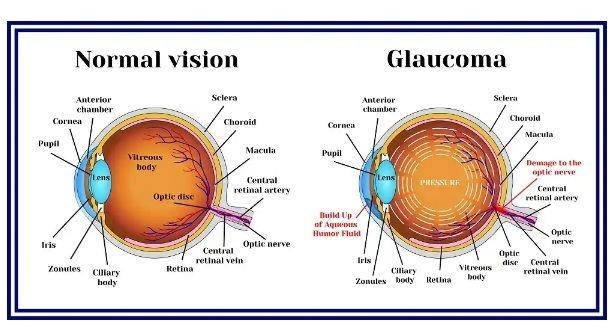
The fluid inside your eye, called aqueous humor, usually flows out of your sight through a mesh-like channel. The liquid builds up if this channel gets blocked or the eye produces too much fluid. Sometimes, experts don’t know what causes this blockage. But it can be inherited, meaning it’s passed from parents to children.
Less common causes of glaucoma include a blunt or chemical injury to your eye, severe eye infection, blocked blood vessels inside your vision, and inflammatory conditions. It’s rare, but eye surgery to correct another condition can sometimes bring it on. It usually affects both eyes, but it may be worse in one than the other.
Glaucoma Risk Factors
It mainly affects adults over 40, but young adults, children, and even infants can have it. African Americans tend to get it more often when more youthful and with more vision loss.
You’re more likely to get it if you:
- Are of African American, Irish, Russian, Japanese, Hispanic, Inuit, or Scandinavian descent
- Are over 40.
- Have a family history of glaucoma.
- Are nearsighted or far-sighted.
- Have poor vision.
- Have diabetes.
- Take certain steroid medications such as prednisone.
- Take certain drugs for bladder control or seizures, or some over-the-counter cold remedies.
- Have you had an injury to your eye or eyes.
- Have corneas that are thinner than usual.
- Have high blood pressure, heart disease, diabetes, or sickle cell anaemia.
- Have high eye pressure.
Types of Glaucoma
There are two main kinds:
Open-angle glaucoma: This is the most common type. Your doctor may also call it wide-angle glaucoma. The drain structure in your eye (called the trabecular meshwork) looks fine, but the fluid doesn’t flow out as it should.
Angle-closure glaucoma: This is more common in Asia. You may also hear it called acute or chronic angle-closure or narrow-angle glaucoma.
Your eye doesn’t drain like it should because the drain space between your iris and cornea becomes too narrow. This can cause a sudden buildup of pressure in your eye. It’s also linked to farsightedness and cataracts, a clouding of the lens inside your eye.
Less common types of glaucoma include:
Secondary glaucoma is when another condition, like cataracts or diabetes, causes added pressure in your eye.
Normal-tension glaucoma is when you have blind spots in your vision, or your optic nerve is damaged even though your eye pressure is within the average range. Some experts say it’s a form of open-angle glaucoma.
Pigmentary glaucoma: With this form, tiny bits of pigment from your iris, the colored part of your eye, get into the fluid inside your eye and clog the drainage canals.
Glaucoma Symptoms
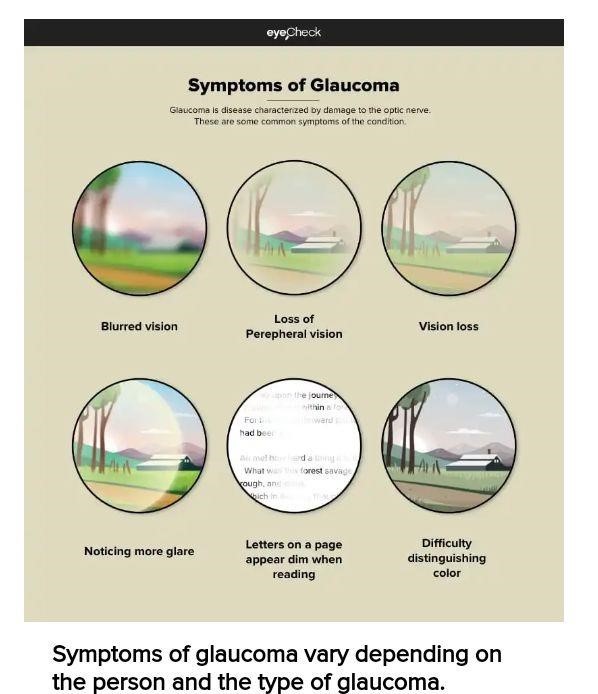
Most people with open-angle glaucoma don’t have symptoms. If symptoms do develop, it’s usually late in the disease. Glaucoma is often called the “sneak thief of vision.” The main sign is typically a loss of sight or peripheral vision.
Symptoms of angle-closure glaucoma usually come on faster and are more prominent. Damage can happen quickly. If you have any of these symptoms, get medical care right away:
- Seeing halos around lights
- Blurred vision
- Loss of peripheral vision
- Glare
- Difficulty distinguishing color
- Vision loss
- Redness in your eye
- Eye that looks hazy (particularly in infants)
- Upset stomach or vomiting
- Eye pain
Glaucoma Diagnosis
Glaucoma tests are painless and don’t take long. Your eye doctor will test your vision. They’ll use drops to widen (dilate) your pupils and examine your eyes.
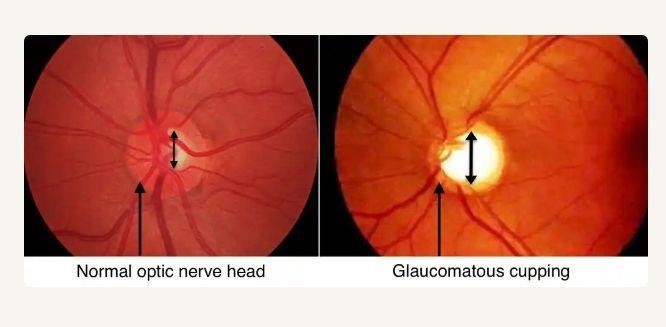
They’ll check your optic nerve for signs of glaucoma. They may take photographs so they can spot changes on your next visit. They’ll do a test called tonometry to check your eye pressure. They may also do a visual field test to see if you’ve lost peripheral vision.
If your doctor suspects glaucoma, they may order special imaging tests of your optic nerve.
Glaucoma Treatment
Open-angle glaucoma is most often treated with combinations of eye drops, laser trabeculoplasty, and microsurgery. Doctors tend to start with medications, but early laser surgery or microsurgery could work better for some people.
Eye drops either lower the creation of fluid in your eye or increases its flow, lowering eye pressure. Side effects include allergies, redness, stinging, blurred vision, and irritated eyes. Some glaucoma drugs may affect your heart and lungs. Because of potential drug interactions, tell your doctor about any other medical problems or medications you take. Also, let them know if it’s hard to follow a regimen involving two or three different eye drops or if they have side effects. They may be able to change your treatment.
Oral medication: Your doctor might also prescribe the medication you can take by mouth, such as a beta-blocker or a carbonic anhydrase inhibitor. These drugs can improve drainage or slow fluid creation in your eye.
Laser surgery: This procedure can slightly raise the fluid flow from your eye if you have open-angle glaucoma. It can stop fluid blockage if you have angle-closure glaucoma. Procedures include:
- Trabeculoplasty. This opens the drainage area.
- Iridotomy. This makes a tiny hole in your iris to let fluid flow more freely.
- cyclophotocoagulation. This treats the size of the middle layer of your eye to lower fluid production.
Microsurgery: In a trabeculectomy procedure, your doctor creates a new channel to drain the fluid and ease eye pressure. This form of surgery may need to be done more than once. Your doctor might implant a tube to help drain fluid. This surgery can lead to temporary or permanent vision loss and bleeding or infection.
Minimally invasive glaucoma surgeries (MIGS): This newer, less invasive form usually requires tiny openings and uses devices you can’t see with the naked eye. It’s generally faster and safer but won’t lower pressure by quite as much. The procedure can also be done simultaneously with other systems, like cataract surgery.
Open-angle glaucoma is most often treated with combinations of eye drops, laser trabeculoplasty, and microsurgery. Doctors tend to start with medications, but early laser surgery or microsurgery could work better for some people.
Acute angle-closure glaucoma is usually treated with a laser procedure.
Infant or congenital glaucoma: meaning you’re born with it — is usually treated with surgery because the cause is a problem with your drainage system.
Tips for Living with Glaucoma
Glaucoma is a lifelong condition and needs continual follow-ups with your eye doctor. There are other things you can do to help keep your eyes healthy.
Get moving: Regular exercise may help lower eye pressure and keep blood flowing to the nerves in your eye. Some activities can raise the pressure, so talk to your doctor about the best exercise program.
Eat healthily: Enjoy a healthy, well-rounded diet. It won’t keep your glaucoma from worsening, but it’s vital to keeping your body and eyes healthy. Some studies suggest that food high in antioxidants can help when you have glaucoma. Eat more nutrient-rich foods like:
Take your medicine: Take your drops or pills precisely as directed. Set a reminder on your phone or watch to avoid forgetting. Missing your meds could make your glaucoma worse.
Careful with contacts: You should be able to continue wearing contact lenses if you use medicated eye drops. But you may need to use some drugs when you don’t have lenses. Also, some older medications can change your vision prescription. And if you need surgery, it may affect your ability to wear contacts.
Don’t smoke: Keeping your body healthy is essential, and nicotine takes a toll. Smoking also raises blood pressure and eye inflammation. That can make your risk of diabetes and cataracts go up. Both are risk factors for glaucoma. If you smoke, ask your doctor for advice on how to quit.
Watch your caffeine: Watch how much soda, coffee, and tea you drink. Too much caffeine can raise your eye pressure. One study found that just a cup of coffee could significantly increase the pressure in your eye for up to 90 minutes.
Elevate your head: Use a wedge pillow when you sleep. It’ll keep your head raised just a little. That should help lower your eye pressure.
Drink fluids slowly: Don’t cut back on how much you drink; spread out your beverages throughout the day. If you drink a lot at once, it can strain your eyes. Don’t have more than a quart at one time. Instead, sip small amounts.
Protect your eyes: Wear protective glasses when working in the yard or playing contact sports. Wear goggles when you swim. When choosing makeup,
use non-allergenic brands, and replace items often. Wear sunglasses outside, especially in summer or around high-glare surfaces like sand, snow, and water. When you have glaucoma, your eyes can be susceptible to glare.
Don’t rub: Glaucoma and medicine might make your eyes feel itchy. But fight the urge. You can scratch them and make things worse. Ask your doctor if you can use drops to treat dryness.
Drive safely: Most people with glaucoma can still drive if they pass their state’s vision test. But your ability to go will depend on how much vision has been lost. Some people with advanced glaucoma can get their licenses renewed with restrictions. Ask your doctor about whether driving will be a concern for you.
Glaucoma Prevention
You can’t prevent glaucoma. But if you find it early, you can lower your risk of eye damage. These steps may help protect your vision:
- Have regular eye exams. The sooner your doctor spots the signs of glaucoma, the sooner you can start treatment. All adults need to be checked for glaucoma every 3 to 5 years. If you’re over 40 and have a family history of the disease, get a complete eye exam from an eye doctor every 1 to 2 years. If you have health problems like diabetes or are at risk of other eye diseases, you may need to go more often.
- Learn your family history. Ask your relatives whether any of them have been diagnosed with glaucoma.
- Follow your doctor’s instructions. If they find that you have high eye pressure, they might give you drops to prevent glaucoma.
- Exercise. Do moderate activity like walking or jogging at least three times a week.
- Protect your eyes. Use protective eyewear when playing sports or working on home improvement projects.
REFERENCES
- National eye institute. “Glaucoma: symptoms, causes, and treatment.”
- Mayo clinic:
Glaucoma – Diagnosis and treatment – Mayo Clinic
Glaucoma: Causes, Types, Symptoms, Diagnosis, and Treatment (webmd.com)
- “Marijuana and Glaucoma.” American Academy of Ophthalmology, 6 May 2020.
- “The Effects of Marijuana on Vision.” American Academy of Ophthalmology, 26 Feb 2021.
Tips & Prevention – American Academy of Ophthalmology (aao.org)
- “Marijuana and Medicine: Assessing the Science Base.” Institute of Medicine (US) Committee on Substance Abuse and Committee on AIDS. National Academies Press (US) 1999.
Appendixes – Marijuana and Medicine – NCBI Bookshelf (nih.gov)
- American Academy of Ophthalmology (2020). Glaucoma: What you Should Know-Retrieved.
Diseases & Conditions – American Academy of Ophthalmology (aao.org)
- Bright Focus Foundation: “9 Tips for Healthy Living with an Eye Disease.”
- International Journal of Clinical Nutrition.
